WHAT IS IT?
Nuclear medicine imaging, also referred to as a nuclear medicine scan or molecular imaging, is a procedure that provides detailed pictures of chemical or biological processes in the body and may be part of a diagnostic evaluation of disease. 1,2
Nuclear medicine imaging procedures use radioisotopes/radionuclides or radiopharmaceuticals (sometimes called radiotracers when used for diagnostic imaging) that accumulate or gather in a specific part of your body and give off radiation that is detected or read by special cameras and computers to create images.1,2
Nuclear medicine imaging is different from other types of imaging, like x-rays, computed tomography (CT or computed axial tomography [CAT]) scans, or magnetic resonance imaging (MRI), which show the structure or anatomy of the body.2
• Radiography (x-rays)
X-rays use electromagnetic radiation, but are not considered nuclear medicine.3
• CT (or CAT) scans
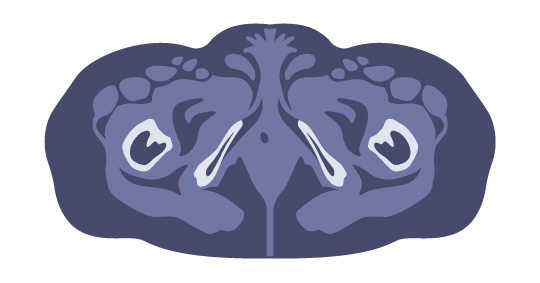
CT scans use a narrow x-ray beam that circles around 1 part of your body to provide a series of images from many different angles that are used by a computer to create a cross-sectional picture.4
• Magnetic Resonance Imaging
MRI scans use a large magnet, radio waves, and a computer to create a detailed, cross-sectional image of internal organs and structures.5
HOW DOES IT WORK?
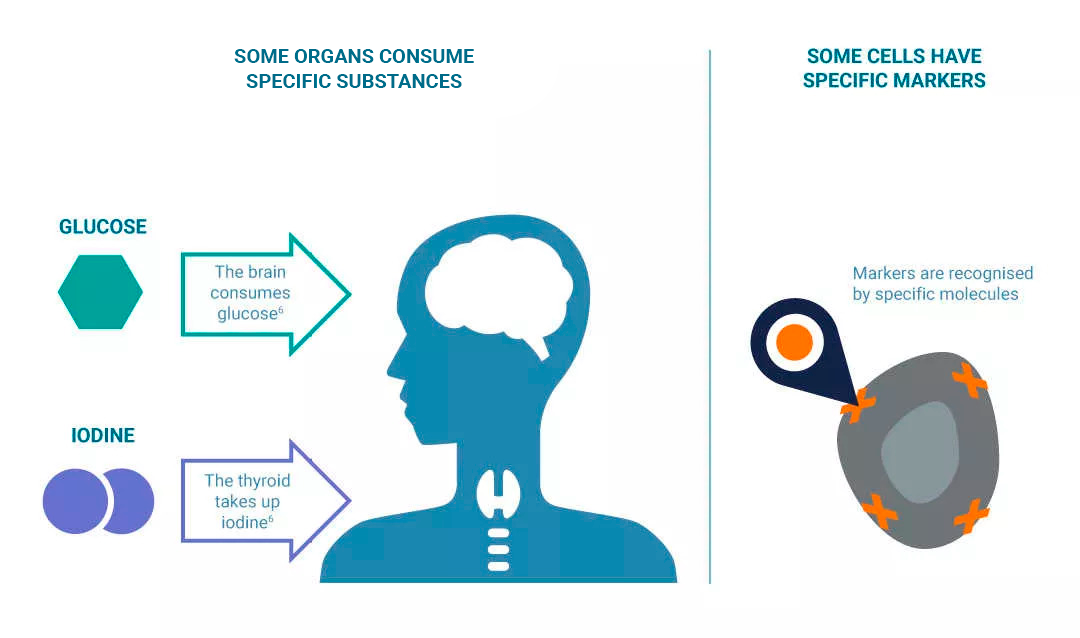
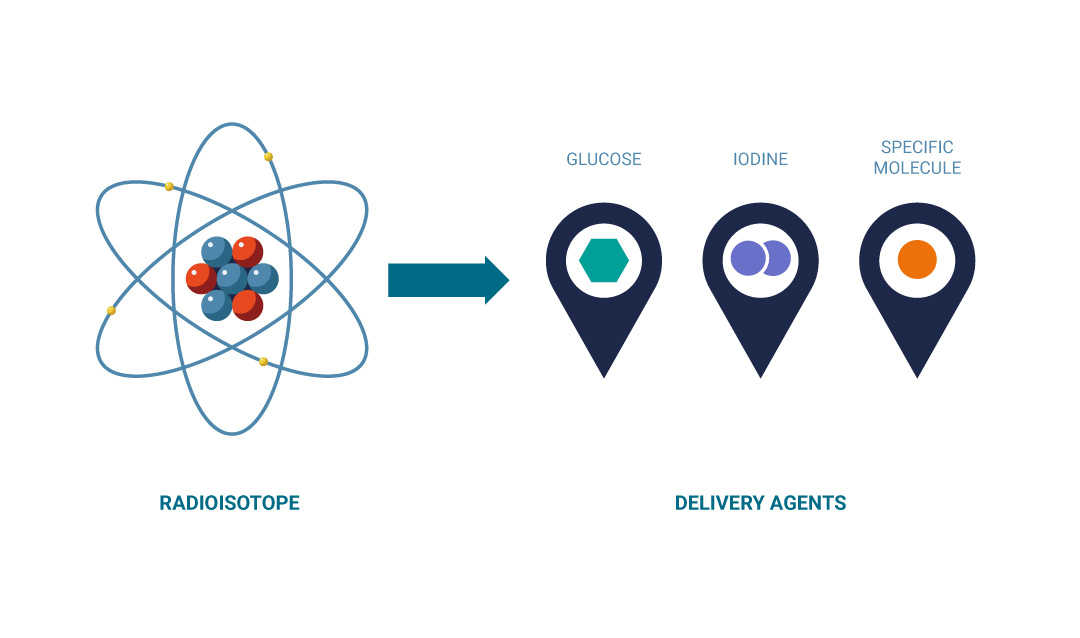
In nuclear medicine imaging, a radiopharmaceutical is chosen for its ability to reach a specific area of interest in the body.
A radiopharmaceutical can either be naturally absorbed by the organ or tissue of interest or designed to connect or bind to a specific cell marker or identifier.1
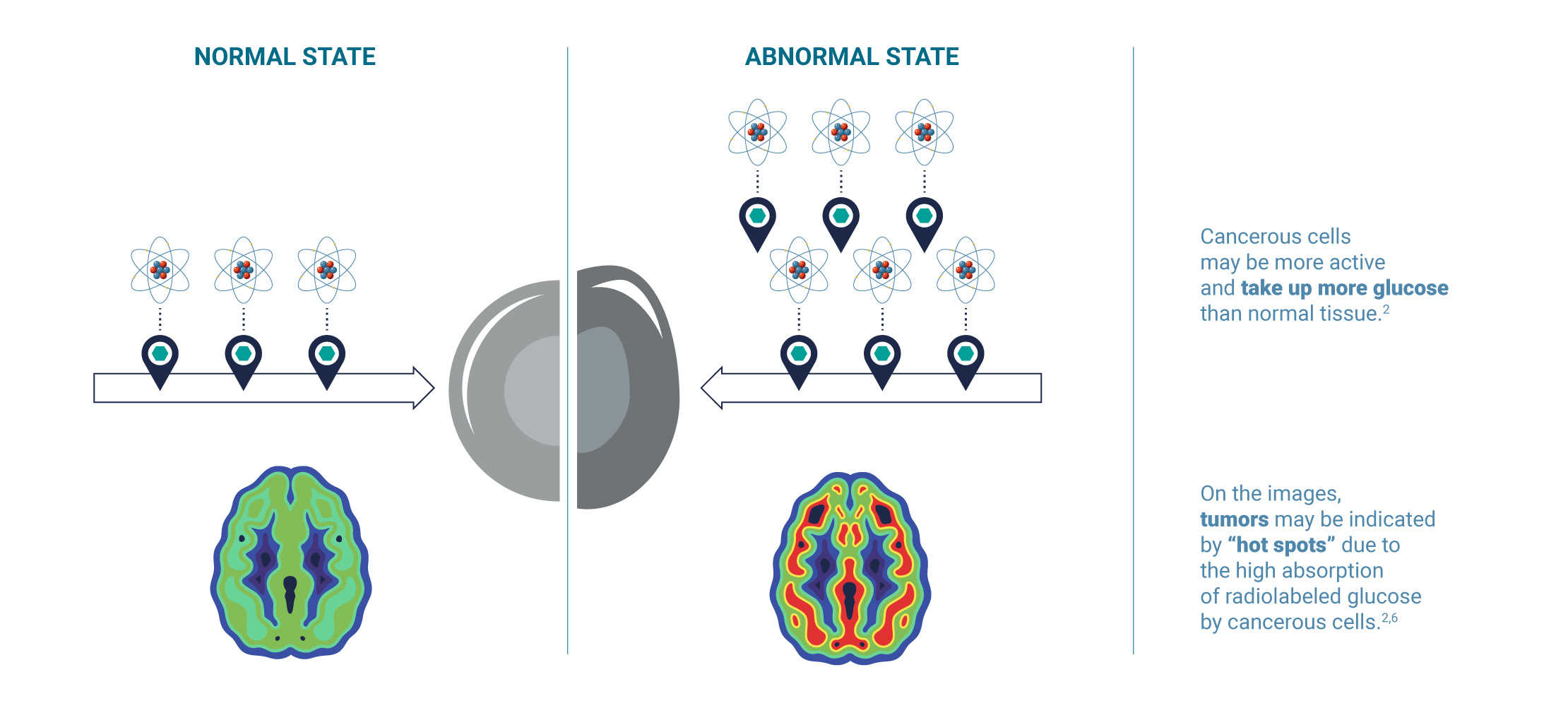
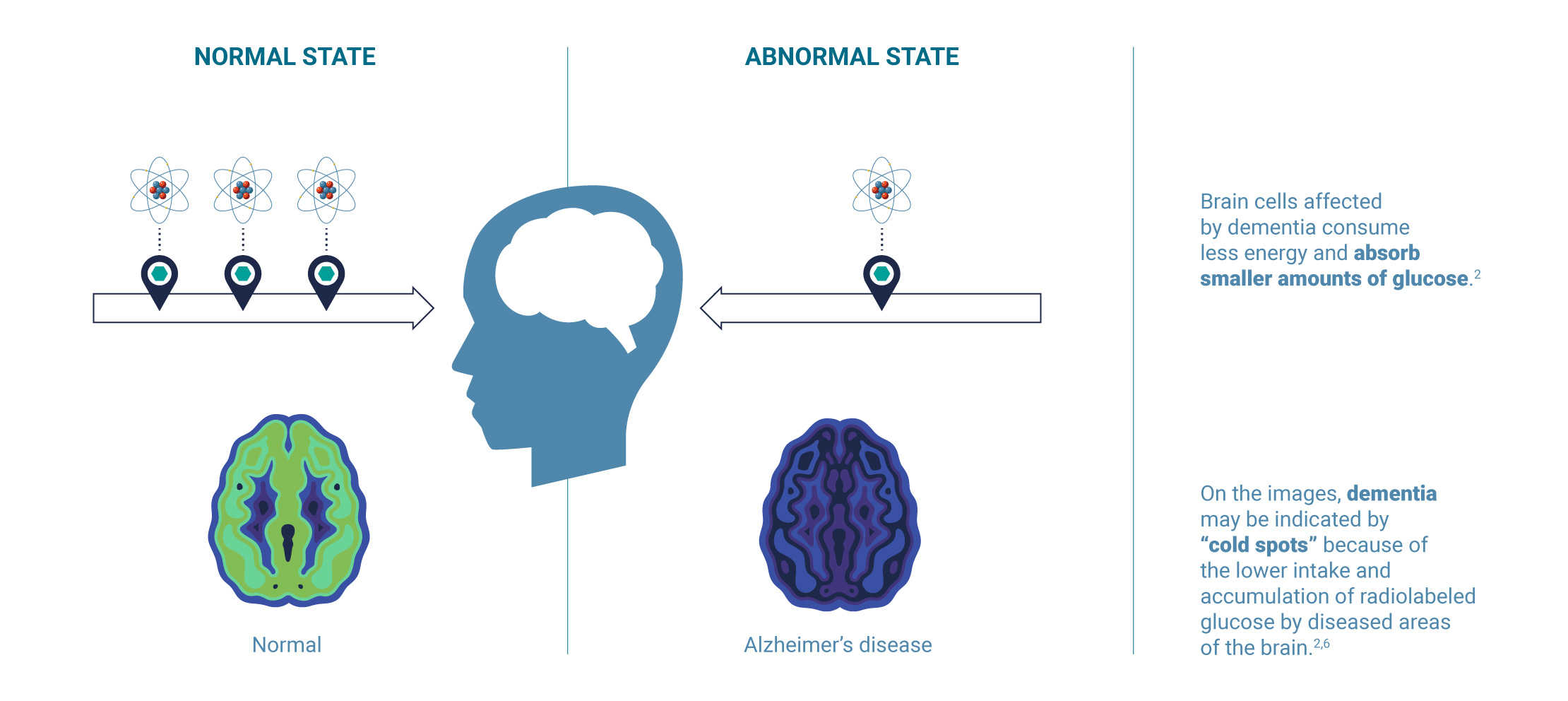
Every cell and organ in your body requires different substances and sources of energy to function.6 When disease occurs, the chemical processes inside living cells begin to change.2 Using this knowledge, scientists have developed radiopharmaceuticals to image these different types of processes.
For example, cancerous cells require a lot of glucose (a type of sugar) for energy and may be more active and take up more glucose than normal tissue. Another example would be brain cells, which also consume glucose, but when affected by dementia consume less energy and absorb smaller amounts of glucose.1,2 The distribution pattern of the radiopharmaceutical used to image the uptake of glucose would therefore provide information on whether an organ or tissue being imaged is acting normally or not.2
Example 1: Imaging cancer
Example 2: Imaging dementia
In nuclear medicine imaging procedures:
• A radiopharmaceutical is administered or given to a patient (by injection, swallowed, or through a catheter tube inserted into the body)2,6,7
• It searches for, travels to, and accumulates in a specific target organ or attaches to specific types of cells2,6
• Diagnostic techniques or methods in nuclear medicine typically use radiopharmaceuticals, which give off gamma rays6
• Special types of cameras pick up or read the patterns of radioactivity from different angles2
• The radioactivity patterns are then processed by a computer to create 2-dimensional (2-D) or 3-D images that show where the radiopharmaceutical travels and where it accumulates2,6
WHEN IS IT USED?
Nuclear medicine imaging is used to help doctors diagnose, evaluate, and monitor progression and treatment in various diseases.2
Nuclear medicine imaging can give doctors certain types of information that is not easily provided by other methods.2
• DIAGNOSIS
Nuclear medicine scans help doctors diagnose disease and determine its location, possibly before symptoms occur or before other diagnostic tests are able to detect chemical changes.2
• EVALUATION OR STAGING
Nuclear medicine scans can allow doctors to determine the extent or severity of the disease.2
• PLANNING TREATMENT
Nuclear medicine imaging can determine the unique properties of a tumor or other disease, enabling your health care team to develop a personalized treatment plan.2
• MONITORING TREATMENT AND DISEASE
Regular nuclear medicine scans can allow your health care team to evaluate if your disease is getting better or worse, or if it has come back.2
This will allow your doctor to determine if your treatment is working and to quickly adapt it depending on how your disease progresses.2

Nuclear medicine imaging may provide your health care team with detailed pictures of biological processes and functions happening inside your body, while other imaging techniques like x-rays, CT scans, or MRIs show structures.2
NUCLEAR MEDICINE SCANS:
• Detect the radiation coming from a radiopharmaceutical that is inside a patient's body8
• Determine the presence of disease based on biological or chemical changes in tissue8
IN CONTRAST, ANATOMICAL OR STRUCTURAL IMAGING PROCEDURES (EG, X-RAYS AND CT SCANS):
• Obtain images by using machines that send radiation through the body8
• Determine the presence of disease based on changes in anatomy or structure8
The example below shows a tumor detected as a “hot spot” in a nuclear medicine scan (A) while the tumor was not detected on an anatomical scan (B).

(A) Nuclear medicine scan shows probable tumor in the form of a “hot spot” (arrow)
(B) CT scan is negative; tumor cannot be detected
Adapted from Townsend DW. J Nucl Med. 2008;49(6):938-55.
WHAT ARE THE DIFFERENT TYPES OF NUCLEAR MEDICINE IMAGING?
In nuclear medicine imaging, there are 3 different types of imaging techniques, all using a special camera that detects the gamma rays given off by different types of radiopharmaceuticals.9,10
• PLANAR SCINTIGRAPHY
Planar scintigraphy is the most basic nuclear imaging procedure.9 The distribution of a radiopharmaceutical is captured by a camera1 detecting the gamma rays being given off from 1 perspective or angle and revealed in a 2-D image.9
These types of scans are mostly used by doctors to screen the whole body for tumors and tumors that have spread to other parts of the body, known as metastases.9
• SINGLE-PHOTON EMISSION COMPUTED TOMOGRAPHY
A SINGLE-PHOTON EMISSION COMPUTED TOMOGRAPHY (SPECT) scan uses a camera that rotates around the patient to detect gamma rays being given off by the radiopharmaceutical and produces a series of 2-D images.9,10 These images are then processed by a computer and converted into a 3-D image of the area being studied.2
SPECT also can be combined with CT or MRI to provide anatomical or structural information.2
SPECT imaging is most commonly used to make a picture of the flow of blood through the coronary arteries and the heart.9-11
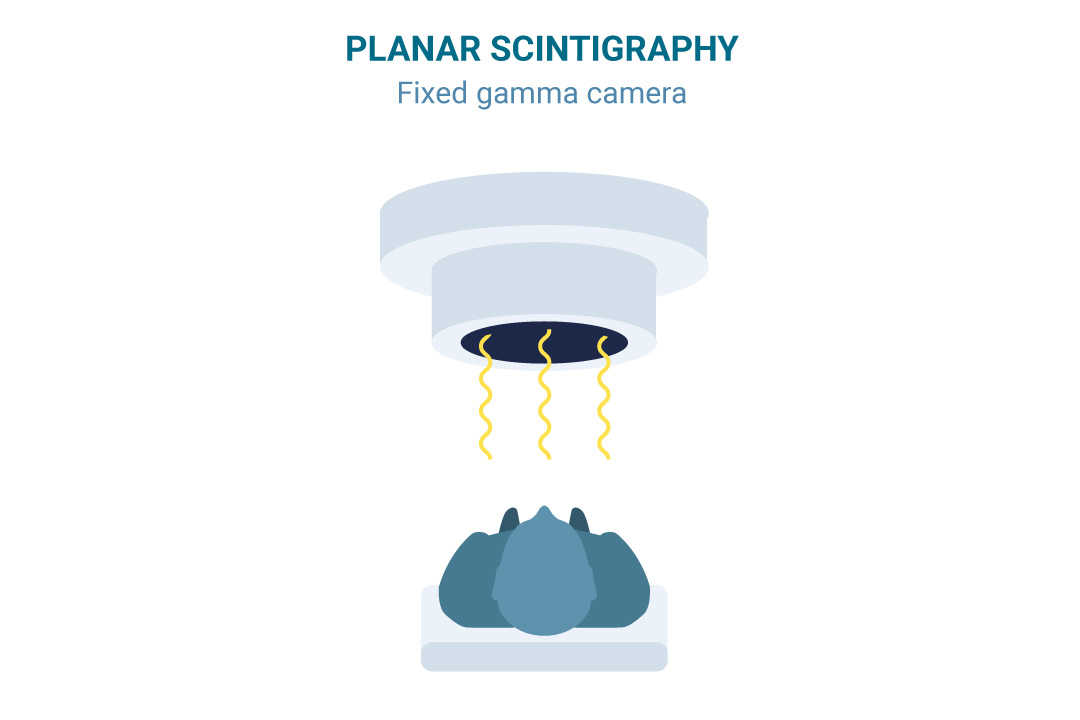
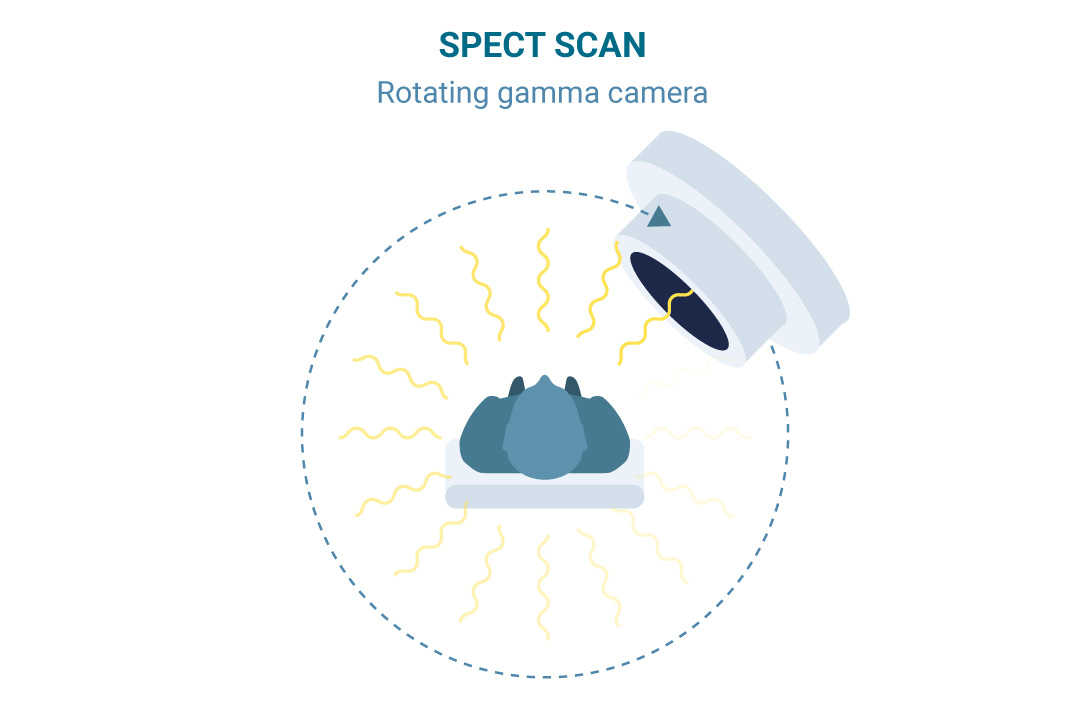
Technetium-99m (Tc-99m) is the most common radioisotope used in planar scintigraphy and SPECT and can
be attached to multiple delivery agents to reach different organs in the body.9,10
• POSITRON EMISSION TOMOGRAPHY
A POSITRON EMISSION TOMOGRAPHY (PET) scanner is a large machine with a round, donut-shaped hole in the middle that looks similar to a CT or MRI unit.1
Multiple rings of detectors inside the machine record the radiation given off from the radiopharmaceutical in your body.1,10 A computer then processes the information into a 3-D image that shows where the radiopharmaceutical accumulates in the area of the body being studied.2
PET scans are used by doctors to detect cancer, brain disorders, heart conditions, and other diseases.12
18F-fluorodeoxyglucose (18F-FDG), a compound combining sugar and the radioisotope fluorine-18,
is one of the most frequently used radiopharmaceuticals in PET imaging.2
Some other radiopharmaceuticals used for PET imaging use different radioisotopes, such as gallium-68, that
are combined with agents that connect or bind to a specific marker on a cell.13
Doctors often use nuclear medicine scans along with other types of anatomical or structural imaging tests for a more complete picture.
CT scans, MRIs, or x-rays are other types of imaging tests that help provide highly detailed images of the body structure.2,14
These types of “combined” imaging procedures involving more than 1 imaging method may be referred to as PET/CT or PET/MRI or SPECT/CT.
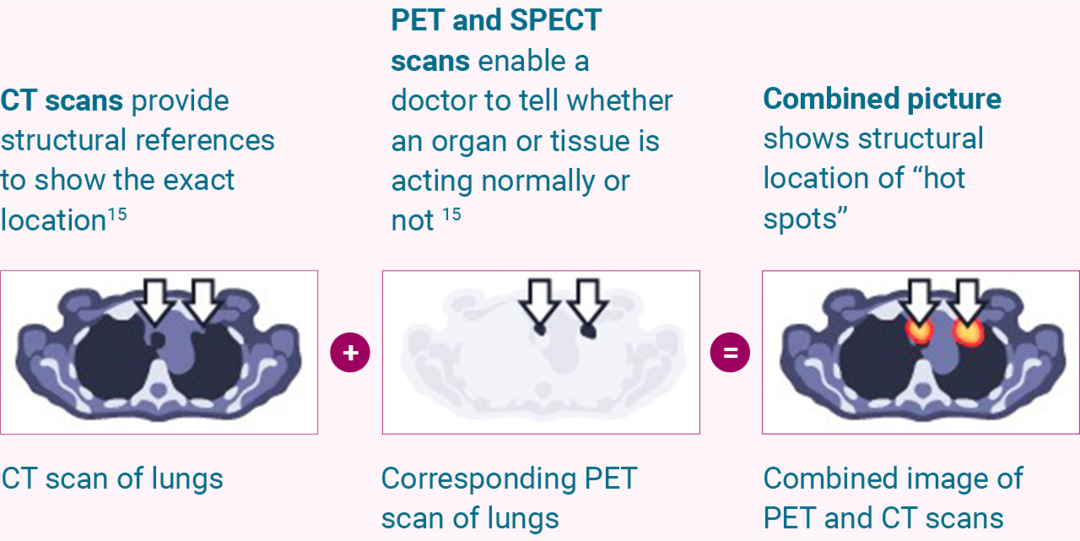
Adapted from Griffeth LK. Proc (Bayl Univ Med Cent) 2005;18(4):321–30.
With the development of new technologies and imaging agents, many of which are in clinical trials, nuclear medicine imaging seeks to continue to deliver improvements to patient care.16
WHAT WILL I EXPERIENCE?
In this section, you will find some answers to the different types of questions that you may have if you need to undergo a nuclear medicine scan.
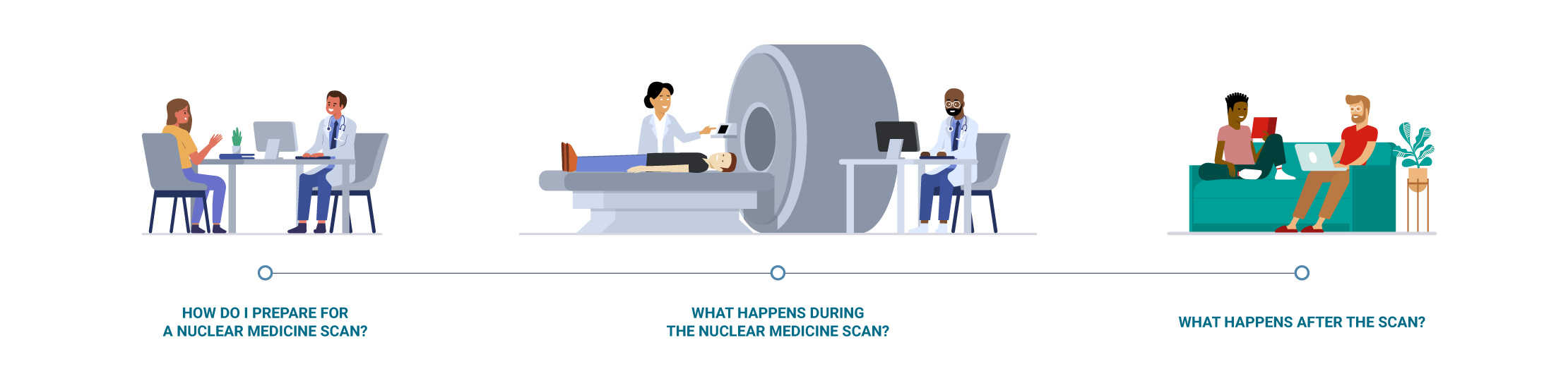
1. HOW DO I PREPARE FOR A NUCLEAR MEDICINE SCAN?
Depending on the type of scan you are having, your health care team will give you specific instructions on how to prepare and what you should avoid before the procedure.
What might I need to avoid before the nuclear medicine scan?
• You may have to remove your jewelery and any other metallic items prior to the scan1,14
• You may need to not eat or drink 2 to 12 hours before the scan14
• You may need to avoid some medicines (prescription and over-the-counter) before the scan14
Can I bring a friend or family member?
• Depending on the facility, you may bring a friend or relative with you; however, this person will not be permitted to be in the same room during the scan. Also, it is best not to have children or a pregnant woman accompany you in order to avoid any potential exposure to unnecessary radiation
• Please be sure to ask your health care team if a friend or family member may come with you to your scan appointment
What key information should I communicate to my health care team?
In general, it is a good idea to communicate any of the following information:
• If you take any drugs – even over-the-counter, vitamins, and herbal supplements1,14
• If you have any allergies14
• If you had any problems with other nuclear medicine scans in the past14
• If you have a implanted medical device such as a pacemaker or a prosthesis17
• If you are or may be pregnant, or if you are breastfeeding1,18
• If you suffer from claustrophobia or a fear of enclosed spaces1
2. WHAT HAPPENS DURING THE NUCLEAR MEDICINE SCAN?
Ahead of the nuclear medicine scan, depending on the type of scan you are having:
• You will be given a radiopharmaceutical anywhere from a few minutes to a few hours or several days before the procedure14
• The radiopharmaceutical may be injected into your bloodstream, swallowed, inhaled as a gas, or administered via a catheter tube inserted into your body1,7
• Most people do not feel pain or unusual discomfort from the administration of a radiopharmaceutical; however, some people may experience pain or swelling at the site where the radiopharmaceutical was injected14
• You may be given a gown to change into or be allowed to wear your own clothing during the scan1,14
• You may be asked to lie on a table or sit in a chair facing the scanner14
• Young children may require gentle wrapping or be given medication to help them relax1
During the nuclear medicine scan:
• The camera or scanner may rotate around you to take a series of images, or it may stay in 1 position and you may be asked to change positions to allow different views to be taken1,14
• You will not feel anything from the scan,17 but you will need to remain very still for brief periods of time while the camera is taking pictures, which may cause discomfort1,14
• The length of time for a scan varies greatly, depending on the type of imaging procedure. Actual scanning time for nuclear imaging procedures can take from 20 minutes to several hours and in some cases may be conducted over several days1
• You may be asked to wait until the technologist checks the quality of the images and, depending on the results, more images may be required1
3. WHAT HAPPENS AFTER THE SCAN?
Can I go back to my normal activities?
• The radiopharmaceutical will naturally be processed and leave your body during the first few hours or days following the scan1
• In many cases, you should be able to resume your normal activities, go home, or go to work shortly after the procedure.1 The dose of radioactive material given is typically low.18 Ask your health care team for specific recommendations based on the type of radiopharmaceutical used
Are there any recommendations I should be aware of?
Your health care team should provide you with any necessary instructions before you leave the facility. Common recommendations include:
• Drinking plenty of water and urinating to help flush the radiopharmaceutical out of your body1,14
• Avoiding being close to children or pregnant women for a certain amount of time after your scan14
• Requesting a letter from your doctor if you will go through security devices, for example at an airport, as they may be sensitive to the radiation levels still present in your body19
Who will follow up?
• A technician will interpret the images and send a report to your referring doctor, usually within a few days. Your health care team will review the results of your scan with you14
As with all medical procedures, it is important for patients to be informed about the particular test or treatment they are receiving.
If you have specific questions or concerns, ask your doctor!
HOW CAN THE RESULTS OF AN IMAGING SCAN IMPACT MY TREATMENT?
Nuclear medicine imaging can enable doctors to develop your individualized treatment plan and adapt or change it as your disease changes over time.

Nuclear medicine imaging offers the potential to identify disease in its earlier stages, which can enable earlier treatment.1

In cases of cancer, the pictures taken with nuclear medicine scans can be used to evaluate or determine the amount of tumor in your body (commonly referred to as disease burden) by showing the unique properties of your tumor(s).10 This may enable your health care team to develop a personalized treatment plan specific to your cancer.10

Nuclear medicine imaging allows your health care team to monitor your disease over time. For example, in the case of cancer, they may be able to see whether the cancer has spread and how it is responding to treatment in order to adapt your treatment course.1

If you need to undergo a particular type of therapy, nuclear medicine scans may provide additional information to help your health care team plan the procedure.1
WHAT ARE THE LIMITATIONS AND POTENTIAL RISKS OF NUCLEAR MEDICINE IMAGING?
As important as they are to diagnosis and treatment monitoring, nuclear medicine procedures do have limitations and risks.
Here are some limitations of nuclear medicine imaging procedures.
• Nuclear medicine imaging procedures can be time-consuming. Depending on the type of procedure, it may take several hours to days for the radiopharmaceutical to accumulate in the area of interest, and imaging may take up to several hours to perform1
• Nuclear medicine scans do not provide very detailed anatomical or structural images on their own, which is why they are often performed in combination with CT or other anatomical imaging techniques to improve diagnosis,6 or followed by x-rays, which are better at showing details of the bone structure14
• Nuclear imaging equipment may not be available at all facilities. The availability of nuclear medicine imaging is limited to clinics with specific licenses and infrastructure20
The following are some complications or risks that may arise from nuclear medicine imaging procedures.

Radiopharmaceutical elimination
• After a nuclear imaging scan, you may give off small amounts of radiation from hours to days depending on the type of radiopharmaceutical used. Ask your health care team about necessary precautions to decrease radiation contamination to those around you10

Radiation level
• Treatment with nuclear medicine therapy will expose you to radiation, which can contribute to your long-term radiation exposure
• Nuclear medicine physicians, medical physicists, and technologists have a responsibility to minimize radiation dose to individual patients, to staff, and to society as a whole, while maintaining the necessary diagnostic image quality. This concept is known as “as low as reasonably achievable” (ALARA)21

Pregnant and breastfeeding women
• In women of childbearing age, pregnancy and lactation status should be known as radiopharmaceuticals can cause fetal harm
• Elective or optional diagnostic nuclear medicine procedures should be delayed until a patient is no longer pregnant
• Because small amounts of the diagnostic radiopharmaceutical may pass in breast milk, breastfeeding should be interrupted for a certain amount of time depending on the radiopharmaceutical used22

Possible adverse or unwanted effects
• Some people may experience pain or swelling at the site where the radiopharmaceutical was injected14
• Allergic reactions to radiopharmaceuticals may occur1,23
• If a patient is claustrophobic, PET/CT scans may cause anxiety
• Nuclear cardiac stress scans might have additional risks because of the stress test performed during the cardiac scan24

Medical history
• The distribution of radiopharmaceuticals in the body can be altered by ongoing medications and prior diagnostic tests (including contrast agents and previously used radiopharmaceuticals)25
• Please be sure to tell your health care team about any medicines you may be taking, other allergies or diseases you may have, and any other treatments or nuclear medicine exams you may have had (such as surgery)
Please be sure to discuss any potential risks with your health care team and ask
any questions you might have.
References:
1. Radiological Society of North America. General nuclear medicine. https://www.radiologyinfo.org/en/info.cfm?pg=gennuclear. Accessed June 6, 2020. 2. Society of Nuclear Medicine and Molecular Imaging. About nuclear medicine and molecular imaging. https://www.snmmi.org/Patients/About/content.aspx?ItemNumber=13294&navItemNumber=13295. Accessed June 4, 2020. 3. Medline Plus. X-rays. https://medlineplus.gov/xrays.html. Accessed July 4, 2020. 4. WebMD. What is a CT scan? https://www.webmd.com/cancer/what-is-a-ct-scan#1. Accessed July 4, 2020. 5. MedicalNewsToday. What to know about MRI scans. https://www.medicalnewstoday.com/articles/146309#what-is-an-mri-scan. Accessed July 1, 2020. 6. World Nuclear Association. Radioisotopes in medicine. https://www.world-nuclear.org/information-library/non-power-nuclear-applications/radioisotopes-research/radioisotopes-in-medicine.aspx. Accessed May 28, 2020. 7. Fettich J, Colarinha P, Fischer S et al. Guidelines for direct radionuclide cystography in children. Eur J Nucl Med Mol Imaging 30(5):B39-44. 8. Society of Nuclear Medicine and Molecular Imaging. SNMMI and safe/beneficial medical uses of radiation. https://www.snmmi.org/ClinicalPractice/content.aspx?ItemNumber=4825. Accessed September 24, 2020. 9. Smith NB, Webb A, eds. Nuclear medicine: planar scintigraphy, SPECT and PET/CT. In: Smith NB, Webb A., eds. Introduction to Medical Imaging: Physics, Engineering and Clinical Applications. Cambridge Texts in Biomedical Engineering. Cambridge, UK: Cambridge University Press; 2010:89-144. 10. Kramer-Marek G, Capala. The role of nuclear medicine in modern therapy of cancer. J. Tumor Biol. 2012;33:629-640. 11. Society of Nuclear Medicine and Molecular Imaging. Single photon emission computed tomography (SPECT). http://www.snmmi.org/Patients/Procedures/Content.aspx?ItemNumber=13529&navItemNumber=13230. Accessed June 6, 2020. 12. Society of Nuclear Medicine and Molecular Imaging. Fact sheet: what is PET? http://www.snmmi.org/Patients/About/content.aspx?ItemNumber=5649&navItemNumber=13293. Accessed June 1, 2020. 13. Smith-Jones PM, Stolz B, Bruns C et al. Gallium-67/gallium-68-[DFO]-octreotide--a potential radiopharmaceutical for PET imaging of somatostatin receptor-positive tumors: synthesis and radiolabeling in vitro and preliminary in vivo studies. J Nucl Med. 1994;35(2):317-325. 14. American Cancer Society. Nuclear medicine scans for cancer. https://www.cancer.org/treatment/understanding-your-diagnosis/tests/nuclear-medicine-scans-for-cancer.html. Accessed June 1, 2020. 15. International Atomic Energy Agency. Radiation protection during PET/CT. https://www.iaea.org/resources/rpop/health-professionals/nuclear-medicine/pet-ct. Accessed June 13, 2020. 16. Society of Nuclear Medicine and Molecular Imaging. Fact sheet: what is nuclear medicine and molecular imaging? https://www.snmmi.org/AboutSNMMI/Content.aspx?ItemNumber=5648. Accessed June 4, 2020. 17. UCLA Health. Frequently asked questions. https://www.uclahealth.org/nuc/faq. Accessed February 17, 2020. 18. AIPES Nuclear Medicine Awareness Group. Will I glow in the dark? http://www.brolbrolbrol.com/NUC/upload/will_I_glow_in_the_dark.pdf. Accessed Feb 2022. 19. Society of Nuclear Medicine and Molecular Imaging. Nuclear medicine and radiation safety. http://www.snmmi.org/Patients/About/content.aspx?ItemNumber=22909. Accessed June 1, 2020. 20. AIPES Nuclear Medicine Awareness Group. Where can I go? http://www.whatisnuclearmedicine.com/Practical-71-Where%20can%20I%20go. Accessed June 13, 2020. 21. SNM Procedure Guideline for General Imaging V6.0. Revised 2010. Available at: https://s3.amazonaws.com/rdcms-snmmi/files/production/public/docs/General_Imaging_Version_6.0.pdf. 22. International Atomic Energy Agency. Preventing unnecessary exposure in diagnostic nuclear medicine. https://www.iaea.org/resources/rpop/health-professionals/nuclear-medicine/diagnostic-nuclear-medicine/unnecessary-exposure. Accessed June 13, 2020. 23. Schreuder N et al. Drug Saf Case Rep. 2019;6(1):4. 24. Mayo Clinic. Nuclear stress test. https://www.mayoclinic.org/tests-procedures/nuclear-stress-test/about/pac-20385231. Accessed September 24, 2020. 25. Callahan RJ, Chilton HM, Ponto JA, Swanson DP, Royal HD, Bruce AD. Procedure guideline for the use of radiopharmaceuticals 4.0. J Nucl Med Technol. 2007;35(4):272-275.
